CY 2026 Proposed Physician Fee Schedule (PFS) Released
On Monday, July 14, 2025, CMS posted the CY 2026 Medicare Physician Fee Schedule (PFS) Proposed Rule.
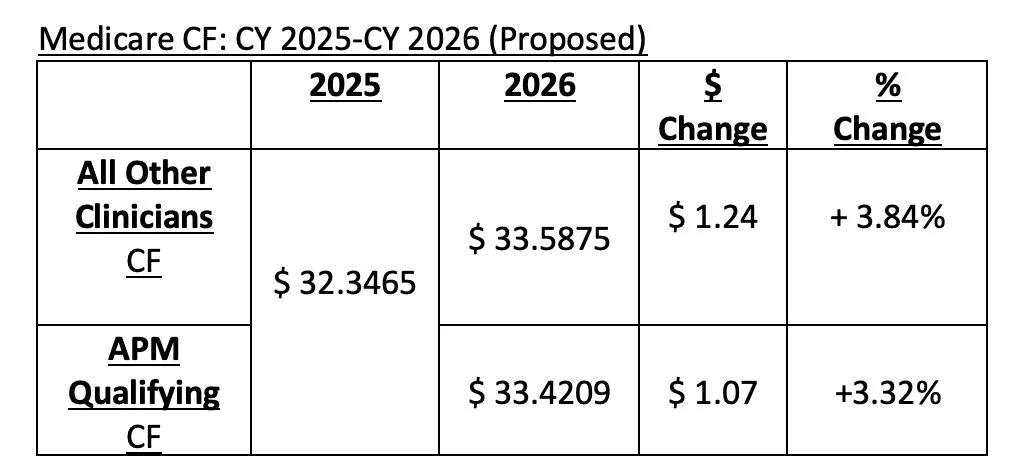
Two Conversion Factors Beginning in 2026
$ 33.5875 (2026 Qualifying APM Participant) and $33.4209 (All Other Clinicians)
As required by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015, beginning in 2026, there will be two conversion factors (CFs).
A proposed CY 2026 CF of $33.5875 for those who qualify based on the Advanced Payment Model (APM) participation was posted. By statute, APM-qualified clinicians receive a 0.75% update beginning in 2026.
A lower proposed CY 2026 CF of $33.4209 for all other clinicians. Clinicians who do not qualify for the APM qualifying CF will receive a 0.25% update beginning in 2026, as required by statute.
Both CFs are also impacted by the +2.50% payment adjustment included in the recent reconciliation legislation, as well as a +0.55% budget neutrality adjustment.
Comments are due September 12, 2025.
A fact sheet summarizing the proposed rule can be found HERE.
A press release on the proposed rule can be found HERE.
Additional updates will be provided as they become available.
For more information or to discuss, please contact:
Sheila Madhani, MA, MPH
Madhani Healthcare Consulting
smadhani@madhani-health.com/202-679-2977